
The sole variable of "disc herniation size" or "disc herniation regression" cannot predict clinical outcomes. If the slipped disc compresses one of your spinal nerves, you may. The correlation between disc regression and improvement of clinical outcomes is a controversial topic, because there are so many variables that influence recovery besides the size of the disc herniation. This is known as a slipped, herniated, or prolapsed disc. This ridge is surrounded by bony openings (foramina) on both sides. At its back, the S1 vertebra has the median ridge or a long bony prominence. S1’s body is characterized by wing-shaped bones on the top on either side, called the alae. The result of this is often neovascularisation and absorption of disc material through phagocytosis and enzyme dehydration.Ĭorrelation between disc herniation regression & clinical improvement S1, or the sacral base, is the upper and wider end of the triangular-shaped sacrum.

Protrusions may be “ focal” or “ broad-based.” (Fardon & Milette, 2001, p.E100).
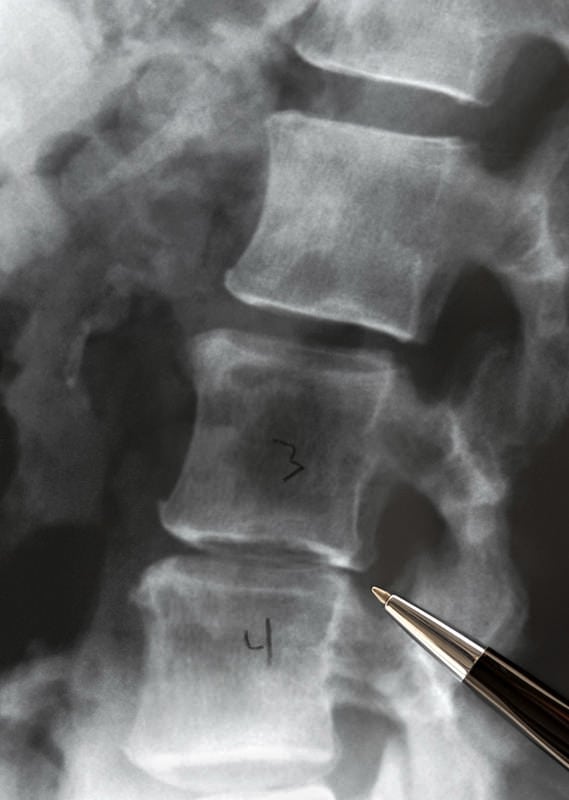
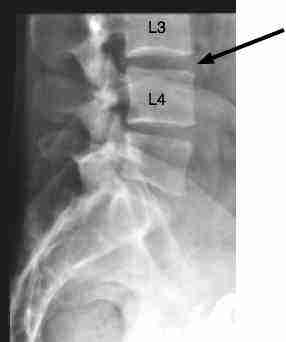
"A disc is “ protruded,” if the greatest plane, in any direction, between the edges of the disc material beyond the disc space is less than the distance between the edges of the base, when measured in the same plane. In 1995, they released a classification that included the following descriptions:īased on this classification one can see that the word bulge can't be used to describe all problems and the word herniation is actually preferred. "Disc herniation is present if there is localized displacement of disc material, and not simply outward overlapping, as is the case with some types of bulging" (Fardon & Milette, 2001, p.E100). In this study, disc herniations were classified using the terms from the 'Combined Task Forces', a committee formed by the North American Spine Society, American Society of Spine Radiology, and American Society of Neurobiology. Their search only included studies that had used conservative treatment. The aim of the systematic review was to investigate the probability of disc herniation regression and complete resolution. X ray only show pelvic tilt and L5,S1 disc space narrowing. In 2014, Chiu and colleagues conducted a systematic review to determine the probability of a spontaneous disc regression. I've recently read this brilliant article that I wish to share with you. While MRI remains a excellent assessment tool, it unfortunately carries the burden of giving patients a beautiful mental image of 'how bad their injury is' and can contribute to negative thoughts about recovery and prognosis. Nevertheless, we have countless studies showing that: people can have disc bulges and be painfree, others can have pain without disc pathology, and some will improve despite MRI imaging remaining the same. We often land up referring for an MRI to confirm clinical diagnosis but, interestingly, we don't often refer for a repeat MRI when people recovery. There is constant debate regarding the clinical necessity of imaging to confirm diagnosis, as well as the potentially harmful effect it may have (mentally). That is some good news!įor many people, medical imaging such as MRI becomes a part of their evaluation at some stage.

A herniation may contain nucleus pulposus, vertebral endplate cartilage, apophyseal bone/ osteophyte and annulus fibrosus.ĭisc herniations can be divided into groups in a variety of ways. Disc herniation refers to the displacement of intervertebral disc material beyond the normal confines of the disc but involving less than 25% of the circumference (to distinguish it from a disc bulge).


 0 kommentar(er)
0 kommentar(er)
